Kaoru Endo, Hozumi Sumitsuji, Takayuki Fukuzumi, Jun Adachi and Toshiyuki Aoki
Department of Dermatology, Habikino Hospital of Osaka Prefecture, Osaka, Japan
Acta Derm Venereol (Stockh)�A77�A432-435�A1997�B
�@ Itching is very important in atopic dermatitis, but the details of itching or scratch movements, especially during sleep at night, have not yet been fully comprehended.
�@We designed a new, simple device ( the Scratch-Monitor ) to evaluate scratch movements at night, and assessed the usefulness of this device by a comparison involving 26 patients and 17 healthy controls.
�@The Scratch-Monitor, a box weighing only 25 g with a pressure-sensor on the bottom, is attached to the back of each hand under a cotton glove and records the number as scratch movements per minute in the case of more than three successive changes of pressure.
�@The Scratch-Monitor indicated that patients with atopic dermatitis scratched more frequently and suffered more severe sleep disturbance than healthy controls. Although the Scratch-Monitor had several problems related to specificity and sensitivity, we concluded that the Scratch-Monitor is a useful tool for evaluating nocturnal itching.
Key words : sleep disturbance; computer analysis; pressure-sensor.
Acta Derm Venereol (Stockh)
T. Aoki, Habikino Hospital of Osaka Prefecture, Department of Dermatology, Habikino 3-7-1, Habikino city, Osaka Prefecture, Japan.
There is no question that itching is of great importance in atopic dermatitis. However, because itching is a subjective sensation, it is difficult to evaluate its level objectively and accurately. If it were possible to measure itching or scratch movements clinically, we could select the best method of therapy for itching in atopic dermatitis. However, the details of itching or scratch movements, especially those during sleep at night, have not yet been fully clarified.
In recent years many devices for measuring the degree of itching have been used. For instance, as part of a patient's self-evaluation, VAS (Visual analogue scale) has been used in Europe (1).
VAS is very useful for evaluating the degree of itching when the subject is awake. Sometimes VAS can be used to make a global evaluation, such as, for itching during the previous week. However, this method depends on the eagerness and intelligence of the subject. Besides its lack of objectivity, VAS cannot be utilized at night when itching is most severe.
To measure scratch movements at night several methods have been reported, that is, muscle potential (2), proximity vibration transducer (3), self-winding watch (3), electromagnetic movement detector (4), paper strain gauge (5), and scratch radar (6). Bergasa et al. (7) have described a computerized scratch-monitoring system based on piezoelectric devices attached to the fingernails.
In this report, we describe a newly designed, simple and easy-to-use device (the Scratch-Monitor) to evaluate scratch movements at night in atopic dermatitis, and assess its usefulness.
MATERIAL AND METHODS
Scratch-Monitor and its problems
The Scratch-Monitor (SM) is a small plastic box, 4.5 cm long, 4.0 cm wide and 1.5 cm high, weighing only 25 g (Fig.1).
The switch button is on the upper side and a button for the marker is on the left side. A pressure-sensor is attached under the SM, by which the number of scratch movements is recorded if there are more than three consecutive changes in pressure at a rate of about once or more/second.
The three levels of sensitivity are available for sensing the change of pressure. We used the medium sensitivity in this study. SM can record data about five days continuously with a dry battery. SM is installed under the cotton gloves on the hand back and is taped on the front and rear so that it will not move. We use two cotton glove sizes to fit the hands of the different patients.

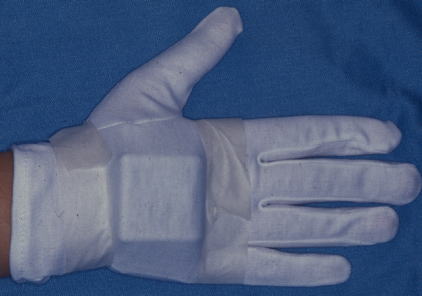
Fig.1 Scratch-Monitor (SM).
�@�@�@�@Two SMs (The right one is No.1 and the left one is No.2) have the same structure. The switch button is on the upper side and a button for the marker is on the left side.
�@A pressure-sensor is under the SM, by which the number of scratch movements is recorded if there are more than three consecutive changes in pressure at a rate of about once or more/second.
�@�@�@�@The data are recorded as the numbers of scratch movements per minute (frequency) at each minute and are analyzed by software installed in a personal computer.
�@However, SM has the following problems related to specificity and sensitivity: The data do not always reflect the scratch movements exactly. When subjects grip or curve their hands, SM sometimes registers a small pressure change.
�@As a result, SM may record a high frequency of movements that are not caused by scratching.
�@�@�@�@When subjects are awake, they may use their fingers for various purposes, thereby causing confusing changes in pressure.
�@SM records all of these movements as scratch movements.
�@Thus, SM should be used only when subjects are asleep. In addition, SM does not always count the number of scratch movements exactly.
Sensitivity Test
�@�@�@Therefore, we investigated SM sensitivity in the following ways : In ten healthy controls, we registered how many times SM recorded scratching on the thigh thirty times .
�@This was repeated ten times at intervals of three minutes.
Subjects
�@�@�@Subjects consisted of 26 inpatients with atopic dermatitis, 14 males and 12 females, mean age 23.5 years (range 14 to 42 years), all fulfilling the diagnostic criteria of Hanifin & Rajka (8), who were in our hospital from October 1993 to April 1994, and 17 healthy controls, 8 males and 9 females, mean age 25.3 years (range 14 to 42 years). �@
�@There were no significant differences in the age or sex distribution between the two groups of subjects.
�@All patients had been hospitalized more than two weeks before our experiment. Prior to installing SM, 15 patients had taken some antihistamines and 11 had not.
�@ At the hospital, 17 patients had been treated with some topical corticosteroids, while 9 had been treated without them.
�@�@�@The clinical severity of AD was determined as follows: 1. A patient with more than 50% of body surface according to the rule of nine affected by atopic eczema is severe; 2. A patient with 10 % to 50 % is intermediate; 3. A patient with less than 10 % or localized eczema is mild.
�@The subjects included 13 severe, 8 intermediate, and 5 mild patients. All the patients were assessed by the same investigator, namely Kaoru Endo, just before SM was installed.
�@�@�@As healthy controls, we chose normal volunteers with no histories of allergic or dermatological diseases.
�@They all had SM installed by their family members in their own home, rather than at a hospital.
�@The study protocol was approved by the ethics committee of Habikino Hospital in September 1993.
�@After the study had been fully explained, informed consent was obtained from all patients and healthy controls.
Method
�@�@�@In this study we used two SMs which had the same structure. Just before the patient went to bed at 21:30, SM (No.1) and SM (No.2) were always installed on the back of the left hand and the right hand, respectively, by a nurse when she used to turn off the lights in our hospital.
�@We directed to have a patient removed SMs and put the switch off by a nurse as soon as the patient woke up.
�@This time only data from the right hand (SM No.2) were used to analyze scratch movements.
�@If a subject was left-handed, SM No.2 was installed on the left hand.
Statistical analysis
�@�@�@Statistical analysis was performed with Stat View (Abacus Concepts, Inc., Berkeley, CA, 1996).
�@Group comparisons were analyzed by the Student's t-test and intergroup comparisons were analyzed by the paired t-test.
�@All p values were two-sided, and were considered significant when they were less than 0.05.
RESULTS
Sensitivity test results
�@�@�@The results are shown. The average number was 22.1�}9.4, and sensitivity was 0.74 (male 0.65, female 0.83).
�@We found that the number of scratch movements recorded by SM had a large dispersion.
�@We considered the following as causes of this dispersion: 1. Differences in hand size, 2. minute differences in the position of the pressure-sensor, 3. differences in the strength of the taping, and 4. differences in the method of scratching.
�@�@�@AD patients scratch in various ways, which are not always registered by SM correctly.
�@For instance, if the subject scratches with only his/her thumb and the sensor does not sense the change in pressure, SM cannot record the movement.
�@�@�@We developed SM to replace the scratch movements with a numerical value to permit evaluation of the itch, rather than to measure the correct frequency of the scratch movement.
�@But for all of these weak points, we concluded that SM would register the scratch movements with sufficient exactitude to permit analysis of nocturnal scratching and to create the possibility of usefulness of clinical application.
�@AD patients complain of itching in the daytime, when tends to be restrained, less frequently than at night.
�@Therefore, we consider that the analysis of nocturnal scratching is equal to that of nocturnal itching or itching itself because there is no restraint on itching.
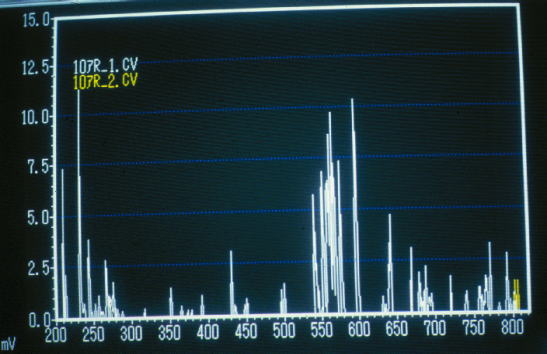
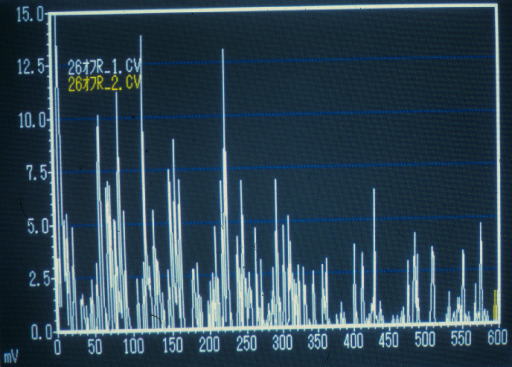
Fig.2-a,b,c are patterns from an AD patient with severe symptoms, an AD patient with intermediate symptoms and a healthy control, respectively. The horizontal axis shows the time course (its unit is a minute.) after the installation of SM. The vertical axis shows the number of scratch movements counted every minute. The expressed number is one tenth the actual number.
Presentation of the typical pattern
�@�@�@Typical patterns from AD patients with severe and intermediate symptoms, and healthy controls are presented in Fig.2 a, b, and c, respectively.
�@The horizontal axis shows the time course, after the installation of SM, in one-minute units.
�@The vertical axis shows the number of scratch movements counted every minute.
�@The expressed number is one tenth the actual number.
�@�@�@The pattern exhibited by the healthy control illustrates very scattered and low peaks, which indicates that the movements of his/her hand is sporadic and sparse during sleep, compared with those of AD patients.
�@This result shows that SM counts very few movements in a healthy control.
�@On the other hand, the pattern exhibited by a severe patient obviously illustrates much denser and higher peaks than that exhibited by an intermediate patient, which indicates that the former moves his hands or fingers more frequently than the latter.
�@We interpret that the series of extremely high peaks, which are caused by grasping fingers and are regarded beyond the ability of scratching, indicate that the patient is awake, since, when we asked these patients, most of them answered that they had been awake around that time.
| Table �T Definition of the term in the analysis of SM |
|
1. 'Asleep' = the first time SM records zero for ten or more minutes, the
beginning of zero 2. 'Awake' = the point when scratch records other than zero begin to just before the removal of SM 3. 'Sleeping time' (min.) = time from 'asleep' to 'awake' 4. 'Pre-asleep time' (min.) = time from the attachment of SM to 'asleep' 5. Three phases of the sleeping period (the early, mid and late period) = three equal parts of sleeping time from 'asleep' to 'awake' 6. 'Scratch rate' = total time with scratch records other than zero (min.)/ 'sleeping time' (min.) 7. 'Minute scratch records' (No./min.) = total scratch records / 'sleeping time' (min.) 8. 'Sound sleeping state' = when SM records zero continuously for more than ten minutes 9. 'Sound sleep rate' = sum of time in the sound sleeping state (min.) / 'sleeping time' (min.) 10. 'Awake bouts' = when a series of scratch records other than zero contains more than fifty or a number other than zero continues for more than five minutes 11. 'Hourly awake number' (No./h.) = number of 'awake bouts' / 'sleeping time' (hours) 12. 'Awake rate' = sum of time in the 'awake bouts' (min.) / 'sleeping time' (min.) |
Definitions in the analysis of scratch movements (Table �T)
�@�@�@In order to evaluate the nocturnal itching of AD with a numerical value, we have to define some terms.
�@'Pre-asleep time' shows if the subject falls asleep easily.
�@'Scratch rate' is used to compensate the low specificity and sensitivity of SM.
�@If the number of scratch movements itself is unreliable, the rate of the total scratching time in the sleeping period can be substituted for the number of scratch movements.
�@'Minutes scratch records' is a numerical value including the demerit of SM. It tends to be affected by high values continually recorded when subjects wake up in the middle of sleeping.
�@Many patients are often disturbed during sleep by itching.
�@We regard sleep disturbance as the other expression of the degree of itching. 'Sound sleep rate', 'hourly awake number', and 'awake rate' show the level of sleep disturbance.
�@We divide 'sleeping time' into three equal parts (early, mid and late periods) to analyze differences of scratch movements between sleeping periods.
�@�@�@Comparison between AD patients and healthy controls (Table �U)
'Sleeping time' was 469.5 minutes in AD patients and 412.6 minutes in healthy controls, but this difference was not statistically significant. 'Pre-asleep time' was longer in AD patients (99.3 min.) than in healthy controls (15.8 min.) with a significant difference, which indicated that AD patients needed more time to fall asleep.
| Table�U Results of the analysis of all patients and healthy controls |
||
| Atopic dermatitis | Healthy control | |
| Sleeping time (min.) | 469.5�}86.7 | 412.6�}84.2 |
| Pre-asleep time (min.) | 99.3�}74.8 * | 15.8�}15.6 |
| Scratch rate | 0.228�}0.116 * | 0.054�}0.033 |
| Minute scratch records | 6.36�}4.96 * | 0.69�}0.65 |
| Sound sleep rate | 0.556�}0.152 * | 0.864�}0.091 |
| Hourly awake number | 0.912�}0.522 * | 0.079�}0.104 |
| Awake rate | 0.135�}0.129 ** | 0.008�}0.011 |
| �@* : p<0.0001, ** : p=0.0003 | ||
�@�@�@'Scratch rate' was 0.228 in AD patients and 0.054 in healthy controls, that is, the former was significantly higher than the latter.
�@As in 'scratch rate', a significant difference was found in 'minute scratch records' which were 6.36 in AD patients and 0.69 in healthy controls.
�@'Sound sleep rate' showed 0.556 in AD patients and 0.864 in healthy controls, a significant difference.
�@A significant difference was also found in 'hourly awake number' and 'awake rate'.
�@�@�@When 'scratch rate' was analyzed for each phase of the sleeping period in AD patients, we found it to be 0.270, 0.234 and 0.183 in the early, mid and late period, respectively.
�@The rate in the late period was found to be significantly lower than that in the early period and that in the mid period (p<0.01).
�@'Minute scratch records' in the mid and late period were also observed to be significantly lower (p<0.05 and 0.001) than that in the early period (9.00, 6.26 and 3.82 in the early, mid, and late period, respectively).
�@The sound sleep rate was the same in all periods.
�@Therefore, we confirmed that AD patients might make the fewest scratch movements before daybreak.
�@This result agrees with our experience in clinical practice.
�@However, 'sound sleep rate' showed no significant difference in the various sleeping periods.
| Table �V Relation of the analyses of those patients with severe and less than intermediate symptoms |
|||
| symptom | |||
| Severe | Less than intermediate |
�@p value�@ | |
| Sleeping time (min.) | 456.2�}74.0 | 482.8�}95.9 | 0.454 |
| Pre-asleep time (min.) | 113.3�}74.1 | 85.3�}72.8 | 0.630 |
| Scratch rate | 0.291�}0.120 | 0.165�}0.065 | 0.004 |
| Minute scratch records | 9.15�}5.03 | 3.57�}2.89 | 0.003 |
| Sound sleep rate | 0.484�}0.152 | 0.627�}0.081 | 0.016 |
| Hourly awake number | 1.316�}0.397 | 0.508�}0.252 | <0.001 |
| Awake rate | 0.201�}0.136 | 0.078�}0.068 | 0.007 |
Comparison of severe and mild AD patients (Table �V)
�@�@�@'Sleeping time' and 'pre-asleep time' showed no differences in the severe and mild groups.
�@But there were significant differences in 'scratch rate', 'minute scratch records', 'sound sleep rate', 'hourly awake number' and 'awake rate'.
�@These results support the conclusion objectively that nocturnal itching is greater in severe patients who suffer from more sleep disturbance.
�@From the results stated above, we conclude that SM is a useful tool for evaluating nocturnal itching in AD.
DISCUSSION
�@�@�@Hagermark and Wahlgren (9) have stated that itching can be recorded and assessed at three different levels : 1. by intraneuronal recording of the activity in the C fibers using microneurography. 2. by recording the scratch movements during sleep. 3. by subjective assessment of the itch sensation.
�@The ways of recording the scratch movements during sleep have all been rather complex and require that the patient stay in a hospital bed.
�@But our device is simple enough to be applied to outpatients as well, which indicates that it would be possible to use it in daily clinical work.
�@Moreover, because of its ease of use, it can be also used to assess the effect of various ways of treating AD.
�@We are going to report an objective evaluation of an anti-histamine agent by using SM.
�@�@�@In this study, no subject dropped out because we selected only submissive patients with full compliance and avoided patients with aggressive characters.
�@In the preliminary study, many patients, about one out of four, were inclined to remove SM by themselves.
�@They told us that they had not been able to sleep well with cotton gloves and SM or had had some pain on their hands, which was caused by the sensor.
�@Therefore, in advance, we asked the subjects to go to bed with cotton gloves for some days.
�@�@�@AD patients often suffer from insomnia because of severe itching at night. Previously, the level of sleep disturbance has been evaluated only by a patient's complaints, scratch marks on the body or blood-stained underwear.
�@However, these methods are not sufficient to assess the insomnia of an AD patient with a numerical value.
�@Our device can also evaluate sleeping conditions at night relatively easily. For instance, a long 'pre-asleep time' indicates difficulty in falling asleep, while a low 'sound sleep rate' indicates waking up many times during the night.
�@These values can be compared before treatment and after treatment for AD.
�@�@�@We designed the SM to objectively evaluate scratching and its clinical application.
�@However, regretfully the number of scratch movements recorded by SM is not always correct for expressing scratching by an AD patient. As mentioned above one of the causes is that an AD patient has various ways of scratching.
�@When scratch movements are monitored by a TV-video system at night, many different styles may be observed in each patient.
�@These styles can be classified into two types of scratch movements, namely sporadic and consecutive.
�@Sporadic scratch movements cannot be measured by SM, which registers only the number of times from more than three consecutive changes in pressure .
�@�@�@SM is the second prototype, which is an improvement on the first one which had a micro switch attached on the tip of each patient's finger stall and a pedometer for registering the data.
�@The first type could register the sum of the number of on and off by scratch movements at night, but we could not analyze the data in detail. Therefore, we expect that improvements in technology will lead to better apparatuses of this type.
ACKNOWLEDGEMENTS
�@�@�@This study was supported by Eisai Co. Ltd. (Tokyo, Japan). We thank Mr. Fumitaka Asano (Gram Corporation, Urawa, Japan) for manufacturing the SMs and the analysis system.
REFERENCES
1. Wahlgren CF, Ekblom A, Hagermark O. Some aspects of the experimental induction and measurement of itch. Acta Derm Venereol (Stockh) 1989; 69: 185-189.
2. Savin JA, Paterson WD, Oswald I, Adam K. Further studies of scratching during sleep. Br J Dermatol 1975; 93: 297-302.
3. Felix R, Shuster S. A new method for the measurement of itch and the response to treatment. Br J Dermatol 1975; 93: 303-312.
4. Summerfield JA, Welch ME. The measurement of itch with sensitive limb movement meters. Br J Dermatol 1980; 102: 275-282.
5. Aoki T, Kushimoto H, Ogushi Y. Computer analysis of nocturnal scratch in atopic dermatitis. Acta Derm Venereol (Stockh) 1980; Suppl 92: 33-37.
6. Mustakallio KK, Rasanen T. Scratch radar (abstract), Skin Pharmacol 1989; 2: 233.
7. Bergasa NV, Jones EA. Management of the pruritus of cholestasis: potential role of opiate antagonists. Am J Gastroenterol 1991; 86: 1404-1412.
8. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh) 1980; 92: 44-47.
9. Hagermark O, Wahlgren CF. Some methods for evaluating clinical itch and their application for studying pathophysiological mechanisms. J Dermatol Sci 1992; 4: 55-62.
Copyright © 2003 Endou Allergy clinic All Rights Reserved